Understanding Depression in Children
Depression is the principal cause of illness and disability in the world. Studies charting the prevalence of depression among children and adolescents report high percentages of youngsters in both groups with depressive symptoms. Depression among children and adolescents is common but frequently unrecognized. It affects 2 percent of prepubertal children and 5 to 8 percent of adolescents.
The clinical spectrum of the disease can range from simple sadness to a major depressive or bipolar disorder. Risk factors include a family history of depression and poor school performance.

What causes depression? Do genetics play a role?
The exact causes of depression are not known. Studies of twins suggest that genes and the environment both play important roles in the development of depression. In addition, an individual’s behaviors and thoughts can play a role in the development and course of depression. As an example, tendencies for depressed people to be pessimistic about the future, themselves, and their surroundings put them at risk for depression.
Chemicals in the brain called neurotransmitters (such as serotonin, norepinephrine, and dopamine) are involved in the onset of depression. Neurotransmitters allow cells in the brain to communicate with each other and play an essential role in all brain functions, including movement, sensation, memory, and emotions. Antidepressants and psychotherapy are designed to reverse abnormal changes in brain chemistry and function.
Many children may feel sad and hopeless from time to time but extreme forms of sadness could be due to depression. Because the symptoms primarily involve thoughts and feelings, depression is called an internalizing disorder. Occasionally being sad or feeling hopeless is a part of every child’s life. However, some children feel sad or uninterested in things that they used to enjoy or feel helpless or hopeless in situations they are able to change. When children feel persistent sadness and hopelessness, they may be diagnosed with depression.
Examples of behaviors often seen in children with depression include:
• Feeling sad, hopeless, or irritable a lot of the time
• Not wanting to do or enjoy doing fun things
• Showing changes in eating patterns – eating a lot more or a lot less than usual
• Showing changes in sleep patterns – sleeping a lot more or a lot less than normal
• Showing changes in energy – being tired and sluggish or tense and restless a lot of the time
• Having a hard time paying attention
• Feeling worthless, useless, or guilty
• Showing self-injury and self-destructive behavior
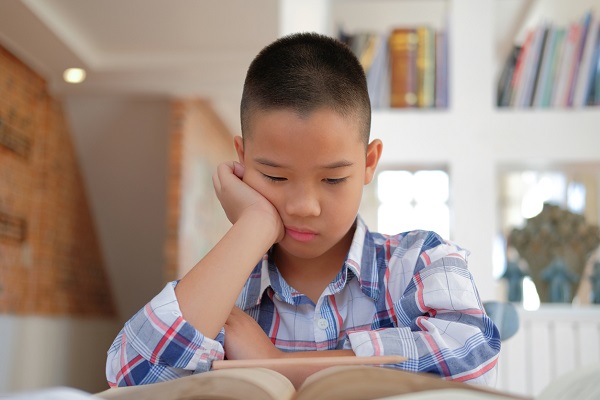
Extreme depression can lead a child to think about suicide or plan for suicide. For youth ages 10-24 years, suicide is among the leading causes of death. Some children may not talk about their helpless and hopeless thoughts, and may not appear sad. Depression might also cause a child to make trouble or act unmotivated, causing others not to notice that the child is depressed or to incorrectly label the child as a trouble-maker or lazy.
Some of the signs and symptoms of depression in children could be caused by other conditions, such as trauma. Specific symptoms like having a hard time focusing could be a sign of attention-deficit/hyperactivity disorder (ADHD). It is important to get a careful evaluation to get the best diagnosis and treatment. The first step to treatment is to talk with a healthcare provider such as your child’s primary care provider, or a mental health specialist, about getting an evaluation. Consultation with a health provider can help determine if medication should be part of the treatment. A mental health professional can develop a therapy plan that works best for the child and family. Behavior therapy includes child therapy, family therapy, or a combination of both. The school can also be included in the treatment plan. For very young children, involving parents in treatment is key. Cognitive-behavioral therapy is one form of therapy that is used to treat depression, particularly in older children. It helps the child change negative thoughts into more positive, effective ways of thinking, leading to more effective behavior.

